Measles Information for Health Care Providers
Description of measles:
Due to a successful vaccination program, measles is rare in the US. However, since 2008, there has been a significant rise in cases due to outbreaks in several states. Clinicians should suspect measles in patients presenting with fever and morbilliform rash and should ask patients about recent travel and other possible exposures.
Measles is a highly infectious, acute viral disease characterized by a prodrome of fever (which can be as high as 103-105 ºF), malaise, cough, coryza and conjunctivitis, which usually occurs 10-12 (range 7 to 21) days after exposure. After 1-4 days of prodrome, an erythematous maculopapular rash develops that usually begins on the face and upper neck and then becomes generalized. Koplik spots (small spots with white to bluish-white centers on an erythematous base) may occur on the buccal mucosa. People who have received vaccinations against measles can have a milder clinical presentation (modified measles) and people who have received antibodies (e.g. newborns with maternal antibodies and people who have received Immune Globulin) can have an atypical presentation (rash progresses in opposite fashion). Complications of measles include bronchitis, pneumonia, encephalitis, and death.
For additional information, refer to CDPH Measles Clinical Guidance.
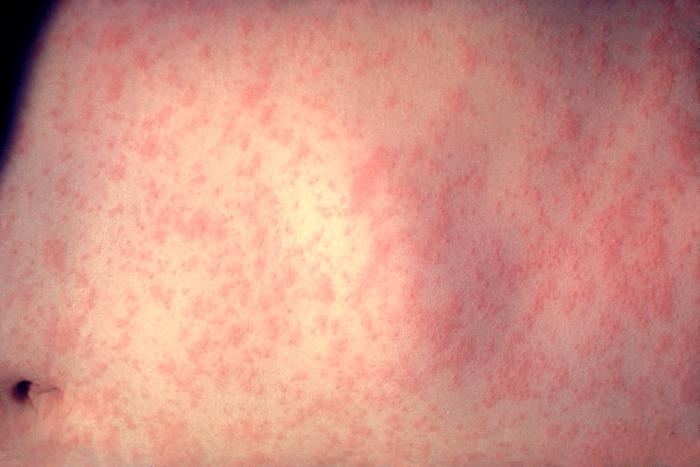
Images
Infection Control:
Measles is transmitted person-to-person via large respiratory droplets and via aerosolized droplet nuclei. People with measles are infectious from 4 days before rash onset to 4 days after rash onset. Airborne precautions should be used immediately with all suspect cases. Patients should be given a surgical mask to wear at all times and should be placed in a private negative air pressure room. If an airborne isolation room is not available, the patient should be placed in a private room with the door closed. Remind triage staff to identify and request assistance for patients with fever and a morbilliform and/or vesicular rash. These airborne precautions should be used for any patient with fever and a morbilliform and/or vesicular rash.
For additional information, refer to CDPH Healthcare Facility Infection Control Recommendations for Suspect Measles Patients.
Post signage that directs patients with fever and rash to notify staff of their symptoms (example). Train staff to immediately implement airborne precautions if measles is suspected.
Notifications and responsibilities:
Immediately report all suspect cases directly to San Mateo County Communicable Disease Control at 650-573-2346. In addition, if the case is or was in the hospital, notify the hospital ICP. Do not wait for laboratory results before notifications.
Diagnosis:
Testing via the Public Health Laboratory system should be pursued immediately for all suspect cases. Do not delay diagnosis by sending specimens to commercial laboratories. Measles can be diagnosed by serology (a positive IgM [collected 4-28 days after rash] or a significant rise in IgG), and by isolation and/or nucleic acid amplification testing from throat or urine specimens. Obtain serum in a serum separator tube, a throat swab on a Dacron-tipped swab placed in viral transport media and a urine sample in any container (does not need to be sterile). After consultation with San Mateo County Communicable Disease Control, specimens should be sent to the San Mateo County Public Health Laboratory at 225-37th Avenue, San Mateo CA 94403 (phone 650-573-2500).
For additional information, refer to CDPH Measles Laboratory Testing Guidance and Measles Testing Algorithm.
Identification of exposed persons (contacts):
All contacts of suspect measles cases should be identified, their susceptibility determined and reported to San Mateo County Communicable Disease Control. In the hospital setting, ICPs will usually coordinate this process. In clinics and offices, clinicians should collaborate with San Mateo County Communicable Disease Control. In non-medical settings, San Mateo County Communicable Disease Control manages identification of contacts to confirmed and suspect cases, and communicates directly with contacts if specific interventions are recommended.
A person is considered a contact if, during the case’s infectious
period, the individual:
a. lived with the case,
b. shared air space with the case for thirty minutes or more, and
was not wearing a mask at the time.
For additional information, refer to CDPH Measles Investigation Quicksheet.
Identification of susceptibility or immunity:
A person is considered susceptible to measles if they answer “No”
to ALL the questions below. A person is considered immune if they
answer “Yes” to any of these questions:
a. Were you born before 1957?
b. Do you have documentation of 2 doses of measles vaccine?
c. Do you have a history of measles with a physician’s
documentation of the infection?
d. Do you have laboratory evidence of measles immunity?
Some contacts to a measles case are unable to produce documentation of receipt of two doses of measles-containing vaccine, and some have received only one dose of measles-containing vaccine. These persons may request measles serology testing (IgG) to assess for immunity. Providing this testing may prevent or shorten the duration of quarantine if immunity to measles can be demonstrated by serologic testing.
Measles, Mumps, and Rubella (MMR) Vaccine Information:
Vaccinate children and non-immune adults, unless contraindicated, according to national guidelines available at www.cdc.gov/vaccines/schedules.
The Centers for Disease Control and Prevention issued a Dear Provider Letter - Adult Measles Vaccination (5/17/19) summarizing the recommendations for vaccination of adults against measles with MMR vaccine. CDPH released recommendations for the vaccination of children and updated recommendations for the vaccination of adults against measles on 5/30/19.
For additional information, refer to ACIP Recommendations for the MMR Vaccine.
Post-exposure prophylaxis (PEP):
If additional cases occur and are promptly recognized, PEP should be pursued for exposed susceptible contacts:
a. Measles-mumps-rubella (MMR) vaccine is recommended as PEP for most susceptible persons aged > 12 months. Administration of MMR is preferable to using Immune Globulin (IG), except as noted below. If administered within 72 hours of initial exposure, MMR or other measles containing vaccine (MCV) may provide some protection. MCV is available in monovalent (measles only) formulation and in combination formulations, such as measles-rubella (MR) and measles-mumps-rubella (MMR) vaccines.
- MMR may be given before 12 months of age but should not be counted as a valid dose. An MMR dose administered before 12 months of age may provide protection from current exposure, but repeat vaccination is still recommended. For young infants, you may wish to consult with a pediatric infectious disease specialist.
- A second dose of MMR may be given any time at least 4 weeks after the 1st dose. It may boost antibody titers in some persons.
b. Immune globulin (IG) can prevent or modify measles in a non-immune person if given within 6 days of exposure. IG is indicated for susceptible contacts at high risk for developing severe measles, including some infants < 12 months old, pregnant women, immunocompromised persons and others for whom the vaccine is contra-indicated. Severely immunocompromised patients and other symptomatic HIV-infected patients exposed to measles should receive IG, regardless of vaccination status because they may not be protected by the vaccine. Infants < 6 months old are usually immune because of passively acquired maternal antibodies. However, if measles is diagnosed in a mother, unvaccinated children in the household who lack evidence of measles immunity should receive IG.
For additional information, refer to CDPH Measles Investigation Quicksheet and CDPH IG for Measles Prophylaxis guidance.